4 Tips to Prevent Stress Injuries in Healthcare Workers on the Frontlines

 Splints, bandages, gauze and bacitracin – basic items of first aid. But what happens to the work of health care providers and emergency responders if they’re injured in ways not visible to the naked eye?
Splints, bandages, gauze and bacitracin – basic items of first aid. But what happens to the work of health care providers and emergency responders if they’re injured in ways not visible to the naked eye?
These “stress injuries” – which can dramatically alter health care providers’ ability to live, work and cope, and almost certainly affect the quality and safety of their work – usually come from four sources, said Richard Westphal, Woodard Professor of Nursing and a psychiatric mental health nurse practitioner in the University of Virginia’s School of Nursing.
Those in the fray of emergency response or on the front lines of a pandemic may experience a threat to their life or a trauma that provokes in them terror, horror or helplessness. They may experience the poignant loss of a cherished person, a way of living, or feel they’ve lost a part of their soul. They may feel great conflict after witnessing something that violates a deeply held belief or value (also called moral distress); and, finally, they may feel deep and debilitating fatigue as a result of all these things, which is an accumulation of stress from multiple sources without time for sufficient rest and recovery.
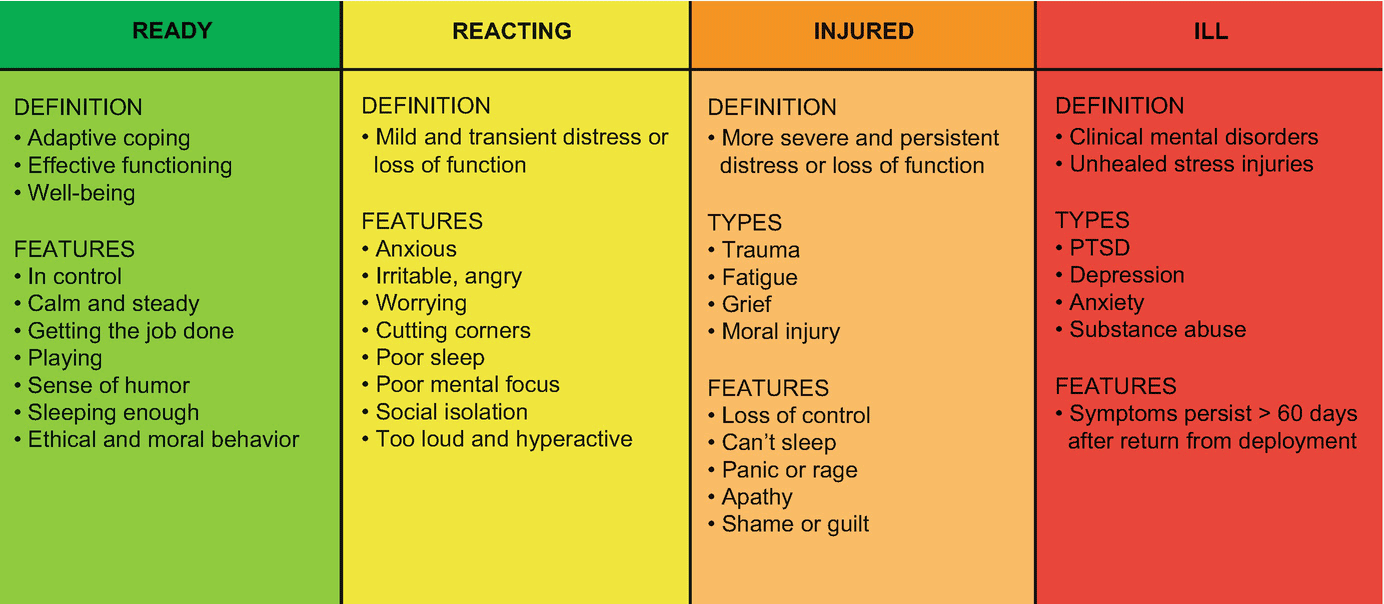
Stress, of course, occurs across a continuum. In Westphal’s work, it’s graded into four colored realms of severity: in the green zone, you’re fit and focused, ready to serve, and if presented with chaos or disaster, you’re confident in your role, know what’s required. Even if confronted with a stressful event, individuals in the green zone can easily get themselves back to a healthy baseline.
But with relentless exposure to high-stress work in challenging environments, like that currently being faced by health professionals on the COVID-19 frontlines, there’s a real danger that responders and caregivers may wander into more dangerous stress territory. And it can happen quickly. In the yellow zone, for instance, people experience anxiety, irritability, and sadness, and act out in ways that affects the quality and compassion of their care. Others may experience persistent distress that impairs their ability to navigate daily life. In the worst cases – considered to be in the red zone, and a sign of a full-blown mental illness – individuals may develop stress injuries that last for weeks or even months at a time – from which they may have difficulty recovering both physically and psychologically.
If the nurse or first responder can’t or won’t recognize their own stress injury and its cascade of ill effects, says Westphal, it’s up to their colleagues or managers to identify the injury and help provide a plotline back to health and functioning. That may mean an honest look at the systems issues adding to the stress, frank but nonjudgmental conversations, and connecting individuals with professional help and resources so they can make their way back into the green zone.
It’s just the kind of scenarios Westphal offers in his stress first aid course, which he’s delivered to firefighters, military personnel, police officers, nurses, physicians, and others over the past 13 years. He insists that helping individuals recognize a stress injury is the first step back to a healthy approach to life, care, and work. Using the simple color-coded approach, as well as the OSCAR stress assessment tool, Stress First Aid peers empowers people on the frontlines with the tools they need to take care of the healthcare workers and emergency responders whose passion it is to take care of us.
The approach – part of UVA Health’s Be Wise campaign – also helps improve working conditions, units’ cohesion and resilience, improves communication, interpersonal behaviors, and gives healthcare and emergency response workers a map to mitigate stress’s effects and improve the workplace and its retention.
“When we support people who are stressed, and those around them,” says Westphal, “we ultimately improve patient care while supporting our own health and wellness, too.”
Learn to Recognize Stress Injuries
Stress injuries happen across a continuum. Psychologically healthy individuals in the green zone are confident and ready in their roles, and when they face a stressful event, they’re able to get themselves back to baseline.
In the yellow, or reacting phase, individuals are in mild distress and feel a level of anxiety, irritability, anger and worry, and begin to lose focus as a result of their stress injury.
More dangerous are the orange and red levels, the point on the stress-injury spectrum where mental illness has taken root. People here are persistently unable to cope with day-to-day life, including work. They may face grief or experience moral distress that inhibits their ability to sleep, makes them feel out of control, panicked, or, on the other end of the scale, apathetic and utterly exhausted.
If you understand these levels, and can recognize them in others and in yourself, you’ll be able to purposefully find your way back to health through the use of peer support, talk therapy, self-care and other resources.
Remember Resilience and Well-Being
School of Nursing faculty members spend a lot of time talking about these topics with students and encouraging them to find a practice that works for them to keep their bodies and minds healthy. Doing that, instructors believe, will reduce the high levels of burnout and professional attrition that plague the health care professions. It’s a sea change from the time when many nursing and medical faculty members were taught that a stiff upper lip was the best defense against experiencing stress injuries.
Some basic rules apply, of course. Rest, good sleep and enough time to recover between shifts is a good starting place. So is avoiding excessive alcohol and eating to self-soothe. Other activities that promote resilience and well-being might include meditation, running, quilting, art, writing, t’ai chi, yoga – any activity that brings calm and meaning to the individual.
Some front-line workers at UVA Health have turned to writing COVID-19-related haiku.
In stressful times, even if individuals feel pressed for time, it’s even more important to carve out moments for these activities. The enormity of the situation calls for your body and mind to be properly functioning.
Instill Calm in Yourself and Others
This is a trait that many first responders and health care workers on the front lines have in abundance: they are good at keeping their breath, their hearts and their hands steady. But it’s not a sign of weakness to feel overwhelmed or panicked. If that happens, there is great benefit to doing a simple breathing exercise using the STOP methodology:
Stop
Take slow deep breaths
Open up and observe how you feel
Proceed with intentional awareness, kindness, wise action
A pause, too, often can bring us back to baseline. If you find you cannot calm yourself, you need to seek help and support from others quickly, before a stress injury takes root.
Look for Connection
This is critical. Whether at work, at home or in virtual spaces, humans crave and need connection. Make sure you’ve got a trusted person to talk you through any difficult cases or issues you’re facing.
With stress injuries, one of the first symptoms of a stress injury is when that health care providers are no longer able to recognize that they’re acting differently, and why peer support and having a “trusted other” is so critically important. Care providers need those who can say, “We’ve been working together for a long time, and I don’t know where your head is lately. So what’s going on?”
Have Confidence in Your Skills – But Don’t Be Afraid to Ask for Help
Nurses, physicians, respiratory therapists, emergency responders, and others are made for emergencies like COVID-19. They’ve trained for this, and understand how high the stakes are in this dramatic moment. But if someone feels themselves slipping into one of the orange or red zones, or observes a colleague slipping, they need to address it directly, in a nonjudgmental way, and ask for help. This is as critical as the work they do on the front lines.
If the nurse or first responder can’t or won’t recognize their own stress injury and its cascade of ill effects, it’s up to their colleagues or managers to identify the injury and help provide a plotline back to health. That may mean an honest look at the issues adding to the stress, frank conversations, and connecting individuals with professional help and resources so they can make their way back into the green zone.
When health care providers support people who are stressed, and those around them, they ultimately improve patient care while supporting their own health and wellness, too.
