$1.2M NIH Grant Uses Tech to Take Aim at Cervical Cancer in Nicaragua


 With a new three-year, $1.2M National Institutes of Health grant, associate professor Emma Mitchell will continue to expand and strengthen the culturally-tailored cervical cancer screening, treatment, and follow-up app and protocol she developed specifically for women in Bluefields, Nicaragua.
With a new three-year, $1.2M National Institutes of Health grant, associate professor Emma Mitchell will continue to expand and strengthen the culturally-tailored cervical cancer screening, treatment, and follow-up app and protocol she developed specifically for women in Bluefields, Nicaragua.
The R21/R33 grant—Remote resilience: Novel applications of mHealth in Nicaragua’s cancer control program—will enable Mitchell to continue development of "Azulado," a novel app she developed with colleague Dr. Rebecca Dillingham that aims to keep women from being lost to follow-up. The second part of the grant will test the app's impact when integrated into a community-based HPV-based primary cervical cancer screening program.
#1 killer
Though largely preventable, cervical cancer is the No. 1 killer of women ages 15 to 44 in Nicaragua
"Emma’s commitment to eliminating cervical cancer inequities in low- and middle-income countries is unwavering," said Jeanne Alhusen, the School's associate dean for research and the UVA Health Professor of Nursing, "and this study will build upon successful collaborations with community partners in Nicaragua."
Over the last decade, Mitchell’s connection to Nicaragua—home to the Central American and Caribbean region’s highest cervical cancer mortality rates, and a country where cervical cancer, which is almost entirely treatable, is the No. 1 cause of death among women ages 15 to 44—has forged alliances with an almost fantastic array of colleagues. She’s well-known in the region, to Nicaragua’s Ministry of Health authorities, at the two universities on the Caribbean coast, and a familiar face and name to the dozens of clinicians who staff clinics.
[VIDEO] 'No More Lost to Follow-Up'
It’s in Bluefields where Mitchell and Dillingham, an infectious diseases expert, professor of medicine, and director of UVA’s Center for Global Health Equity, put cervical cancer in their crosshairs, developing nuanced systems to screen, follow up with, and treat patients who’d developed cervical cancer, which is caused by high-risk genotypes of the human papilloma virus, or HPV.
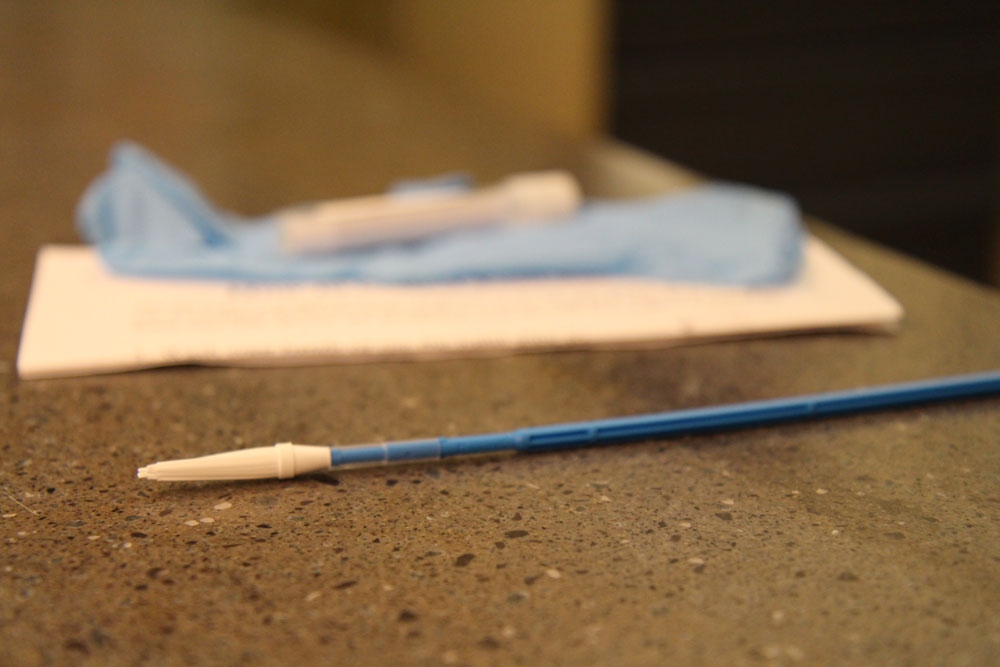
Self-collection HPV tests, for instance—done quickly in the privacy of one’s home—resonated in Bluefields, a region where just one-third of women have ever had a Pap test, but where almost everyone has a cell phone and internet access. With community partners, Mitchell and Dillingham developed the smartphone app Azulado (“blueish” in Spanish, a reference to the region’s diverse 60,000 Mestizo, Black, Caribbean and Indigenous peopl) that is culturally, linguistically, and technologically tailored to women up and down the Caribbean coast.
It also works.


When the pandemic struck, Mitchell’s project infrastructure was largely in place: a local lab to process and diagnose self-collection samples, a method to feed data into Nicaragua’s National Cancer Surveillance System, a protocol for following up with HPV-positive women, and training for rural gynecologists to remove cervical cancer lesions using a smartphone-based colposcope, and a mobile thermo-ablation machine, as well as a low-cost cervical simulator to train them.
“These aren’t processes that occur overnight; they’re not processes that occur when someone from UVA flies to a place and says, ‘This is how you do it.’ You figure out how to do it by taking the time to understand what’s happening, know what partners want to happen next, and how that can be achieved.”
Infectious diseases physician Becca Dillingham, co-creator of Azulado and Mitchell's partner
So, in spring 2020, when nearly 2,000 HPV self-collection kits were received during the first phase of Mitchell’s pilot study, more than 350 HPV-positive women were quickly notified, connected with resources, and urged to take the next steps for treatment. In a moment when the pandemic might have derailed cervical cancer detection and treatment, nearly all of women with cancerous lesions were treated.
The new smartphone app—which debuted in spring 2021—is the critical final piece of Mitchell’s tailored approach. It provides a roadmap and ethos for other resource-limited countries battling cervical cancer looking for best practices, important as the World Health Organization aims to eradicate cervical cancer in the next century.
But while cool tech often gets props, Dillingham insists the study’s success is built on the partnerships and mutual respect Mitchell has built over time.
“We’re modeling the kind of collaboration that’s essential for true change to occur,” Dillingham said. “These aren’t processes that occur overnight; they’re not processes that occur when someone from UVA flies to a place and says, ‘This is how you do it.’ You figure out how to do it by taking the time to understand what’s happening, know what partners want to happen next, and how that can be achieved.”
Mitchell and her development team continue to refine and tailor the app, and, with the new NIH funding, will expand their screening, follow-up, and treatment protocols to communities surrounding Bluefields up and down the Caribbean coastline.
###
