Nursing Hearts
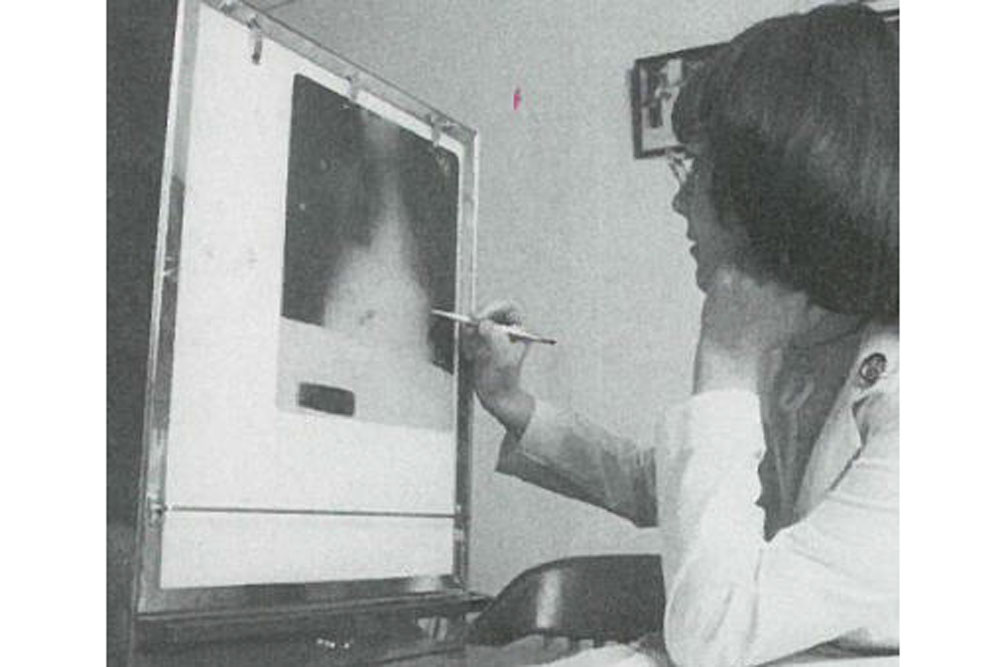
With St. Valentine’s Day’s proximity, today’s flashback offers a look back at the growing specialty of cardiac medicine, and how it fundamentally – and permanently – shifted the role of nurses from subservient caregiver to patient-centered providers.
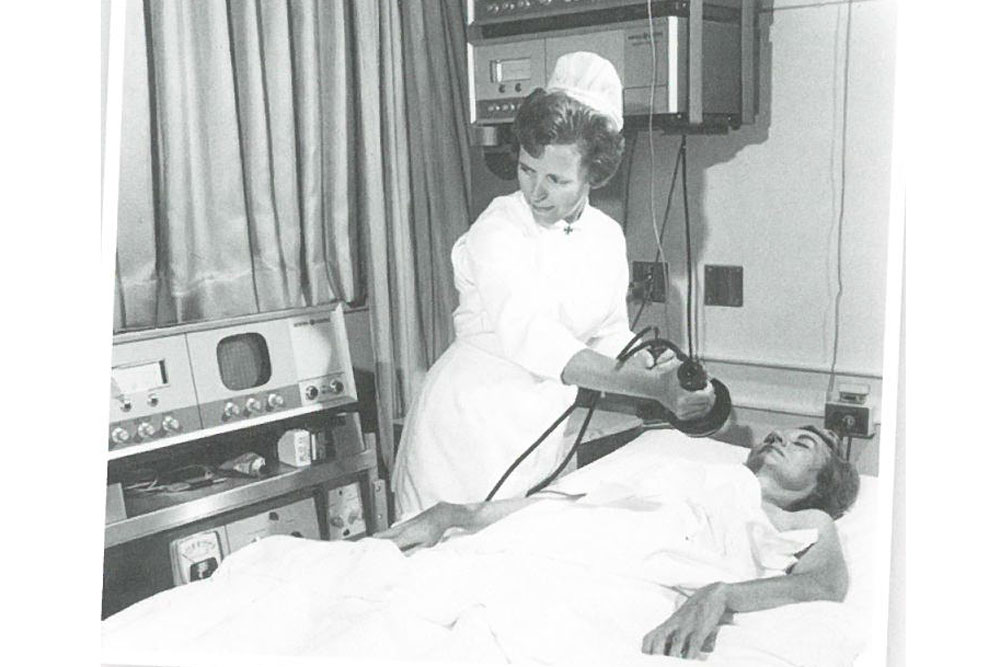
Kansas City's Bethany Hospital established the nation's first Cardiac Care Unit (CCU) in 1962, which had specially trained nurses who not only cared for critically ill patients, but established and managed IVs, did CPR, and closely monitored cardiac patients – skills these nurses mostly learned on the job.

In the mid-1950s, an RN’s ability to establish IVs was determined by state law. But their ability to call for and administer CPR – which requires an ability to read an EKG and understand cardiac rhythms – almost entirely depended on whether it was day or night. If a physician was present during daytime hours, the nurse ceded that role. If a patient needed CPR during the night shift, however, when no MD was around, nurses were authorized to make a clinical judgement and proceed with CPR. Some called it "sundown syndrome."
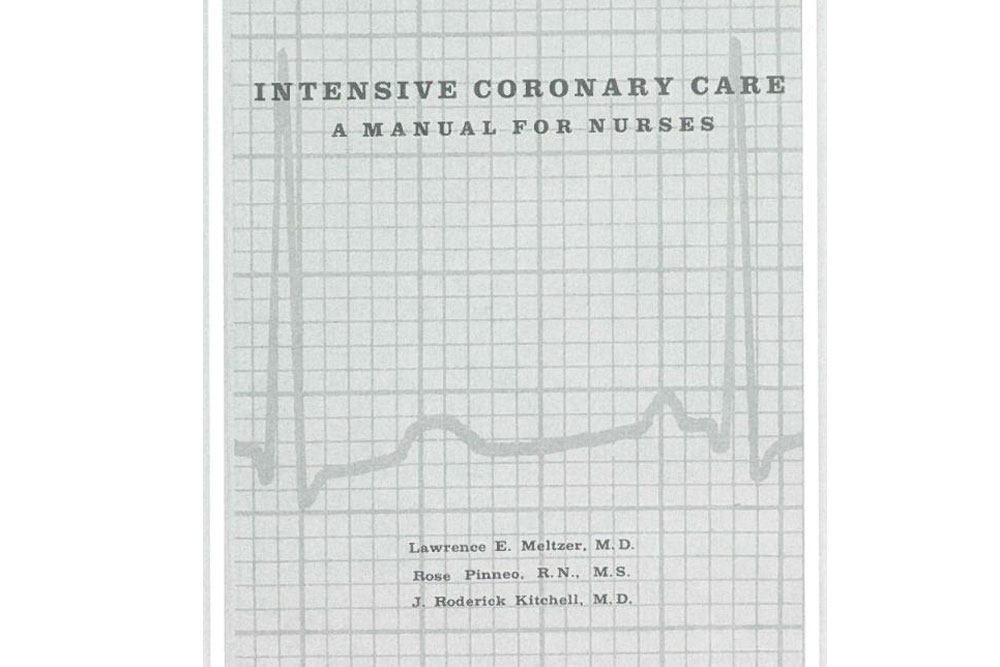
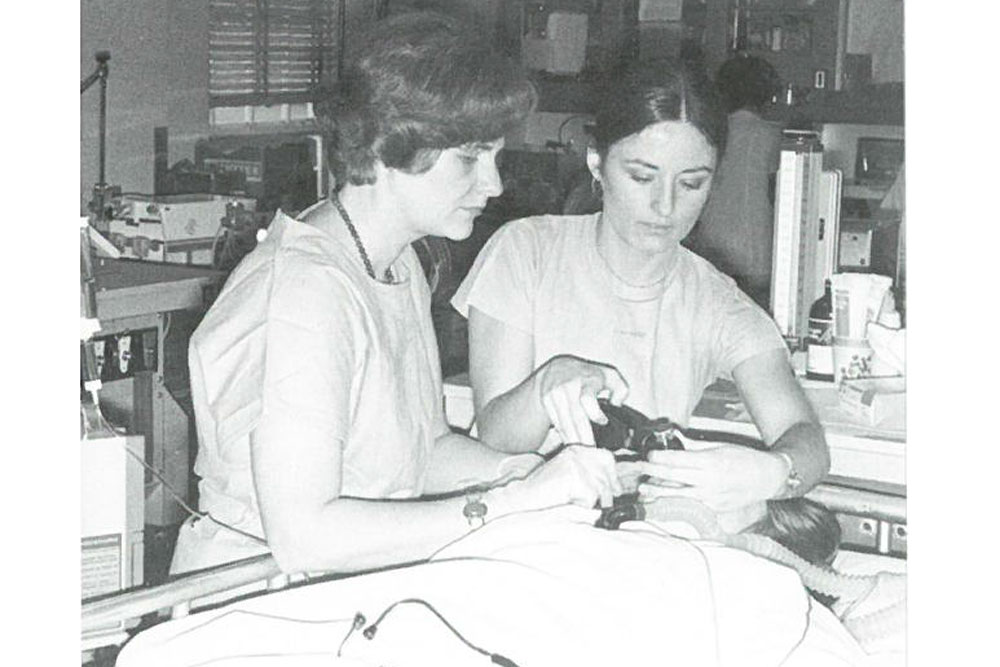
As more CCUs opened, and demand for specially-trained nurses grew, questions about RNs' scope of practice arose. At Philadelphia's Presbyterian Hospital, physicians Lawrence Meltzer and J. Roderick Kitchell, with RN Rose Pinneo, conducted research that found nurses could successfully take on the new, high-level responsibilities of cardiac monitoring, CPR, and cardiac defibrillation. Their resulting work -- Intensive Coronary Care for Nurses: A Manual – helped thousands of nurses learned to interpret EKGs.
These acts of diagnosis and treatment - administering IV medication, identifying cardiac arrhythmia, defibrillating a patient's heart, beginning CPR when it was called for – all "crossed the boundary of physicians’ customary territory," writes professor emerita Arlene Keeling. "The line between medicine and nursing was blurring."
It wouldn’t be long before UVA and other nursing schools would open master’s courses, offering clinical nurse specialists and nurse practitioner degrees, both of which offered RNs a growing level of specialization, increased access for patients, and ever more well-deserved autonomy.
This #FlashbackFriday brought to you by the Bjoring Center for Nursing Historical Inquiry, with special thanks to AAHN President Arlene Keeling, whose book A PROFESSIONAL HISTORY OF NURSING IN THE US provided the basis for this passage (Springer: New York). #histmedicine #histnursing
###
