Taking Aim at Burnout

When Scott Austin, a nurse manager on UVA Health’s COVID unit, sees his coworkers’ faces grimace, hears patients shout, and senses his unit begin to sink under stress, he circulates a text. That “Code Orange” brings everyone—from housekeeping to techs, nurses, and physicians—to a screeching (albeit safe) halt.
To pause. Debrief. Redistribute. Reset.
"I don't want people to roll their eyes and say, 'Oh, not another training session,' because it's not . . . Give it a chance; it'll help you. I promise."
Scott Austin (BSN `18), nurse manager of UVA Health's COVID-19 units, who's taken Wisdom & Wellbeing training
“These are stressful times, so just taking three to five minutes to talk with and listen to team members reminds people that we care about them as human beings, not just as nurses, or techs, or employees doing a job,” said Austin, a UVA clinician for 16 years who has dealt with burned-out staff, mass resignations, and the relentless sickness and death that COVID-19 brings. “Mental health has been a real challenge for many healthcare providers, but as Nightingale said, ‘Little can be done under the spirit of fear.’ Like a lot of people, I was a naysayer early on, but Richard and Peggy have taught me a lot.
“None of us have done anything like this before,” he added, “and I can honestly say that without the 3 West team, Richard, and Peggy, I’m 100% confident that I would’ve failed miserably.”
2/3 of nurses and 40% of physicians
report they're burned out (Dr. Lorna Breen Heroes' Foundation)
It was March 2020 when Austin first called Richard and Peggy—that’s Professors Richard Westphal, the Woodard Professor of Nursing, and Margaret Plews-Ogan, the Brodie Professor of Medicine, who created and co-direct UVA Health’s Wisdom & Wellbeing program—for help. Dozens of times since (connecting by text, phone, at on-unit staff meetings, and pre-shift huddles), they’ve helped clinicians talk, hear, and support one another, guiding teams—not individuals—to support one another as they navigated an unfolding pandemic that’s since claimed millions of lives. The “Code Orange” pause is just one of the lessons Austin’s taken to heart.
Now, with a new $2.14 million grant—part of President Joe Biden’s $103 million American Rescue Plan and the Lorna Breen Act—Westphal and Plews-Ogan will expand their nationally-lauded program in a moment when much of healthcare is on its knees: nearly two-thirds of American nurses and more than 40% of physicians now say they’re burned out, a condition associated with a 200% increased risk in medical errors, as well as higher rates of substance abuse, mental illness, and suicide. Physicians and nurses now kill themselves at twice the rate of the general population.
“COVID has really stripped away the illusion that team members can keep sucking it up, and going back to work,” said Westphal, a psychiatric nurse practitioner. “That has never worked. This is about changing the culture.”



The new grant will enable the expansion of the pair’s Wisdom, Wellbeing, and Peer Support Training program, which places the focus for well-being on healthcare teams, rather than individuals, by teaching them to identify and treat “stress injuries,” occupational wounds caused by trauma, loss, moral distress, and burnout that cripple wellbeing and impact patient care quality and safety. In a unit-by-unit approach, they tap healthcare workers’ core strengths—traits such as stoicism, selflessness, loyalty, and adherence to a moral code—and de-stigmatize language about mental illness. The expanded effort will also give health professionals ways to effectively respond to bias and discrimination from patients and peers, an increasing threat, and to develop, deploy, and sustain robust on-unit practices that collectively boost cohesion by taking aim at stressors large and small: chronic understaffing, overwhelming and unnecessary documentation, and consistently unrealistic goals and expectations.
“Fundamentally,” said Plews-Ogan, “people are not expendable. They are worthy of the attention required to help them be their best.”
“Fundamentally, people are not expendable. They are worthy of the attention required to help them be their best.”
Peggy Plews-Ogan, co-director of UVA Health's WIsdom & Wellbeing program and the Brodie Professor of Medicine
In addition to connecting with more than 8,000 UVA Health staff, 1,100 nursing and medical students, and more than 1,000 rural community health workers (including first responders, school nurses, and mental health counselors across Central Virginia), the new grant also establishes a national Wisdom, Wellbeing, and Peer Support Training collaborative with the Dr. Lorna Breen Heroes’ Foundation, a train-the-trainer model that will further expand Westphal and Plews-Ogan’s model to healthcare communities across the country and around the world.
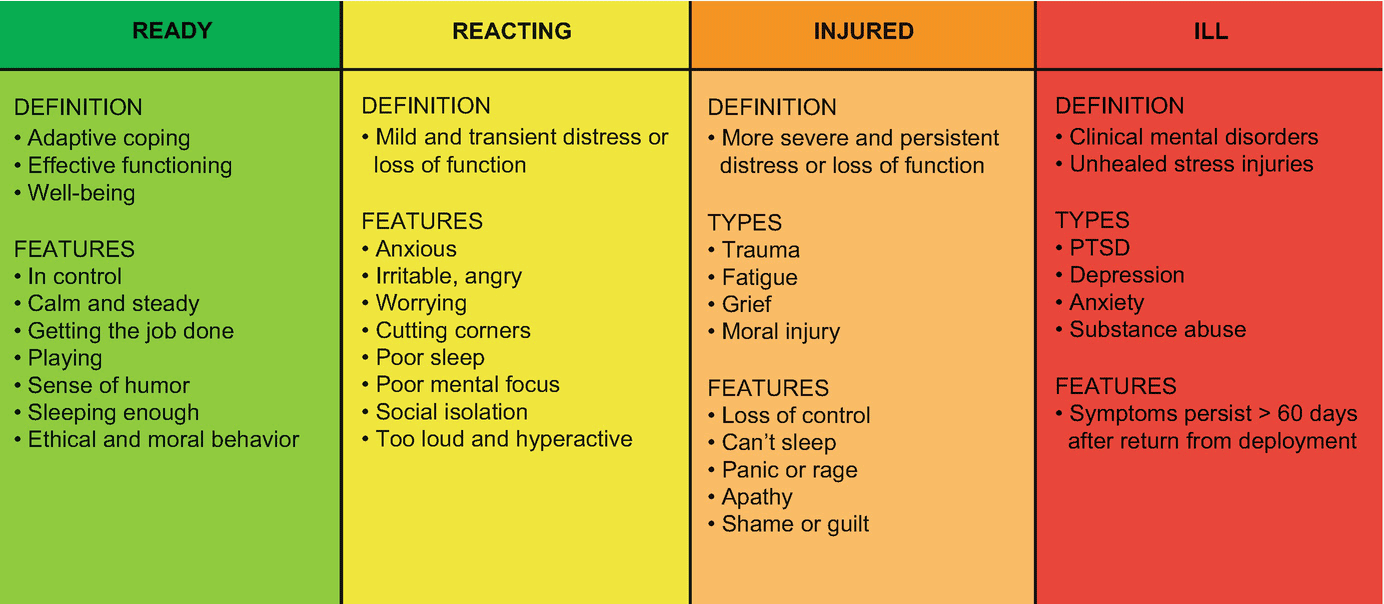
The expansion is the culmination of their life’s work. Westphal led development of the Stress First Aid approach— a system that assesses individuals’ response to stress across a color-coded continuum from green (ready), to yellow (reacting), orange (injured), and red (ill)—while program manager of the Navy’s $117 million psychological health and Traumatic Brain Injury programs from 2007 to 2010—a system still used by military professionals, firefighters, police officers, EMTs, and frontline healthcare workers around the country.
“COVID has really stripped away the illusion that team members can keep sucking it up, and going back to work. That has never worked. This is about changing the culture.”
Professor and NP Richard Westphal, who pioneered the Stress First Aid approach and co-created Wisdom & Wellbeing
Plews-Ogan—whose career has focused on humanism, wisdom in medicine, and the use of positive approaches to improve patient safety and quality—developed and tested many of Wisdom & Wellbeing’s components, including the professionalism coaching program, the “critical events” peer support model, and the Steppingin4Respect framework.
During the pandemic, the Wisdom & Wellbeing team repeatedly delivered wisdom practices and Stress First Aid across UVA Health through on-unit consultations, deployed a resource-rich web site, and expanded the network of trained peer support team members, work that proved powerful. A pre-COVID pilot in the Surgical Trauma ICU, for example, reduced turnover by 54% after the Wisdom and Wellbeing principles were rolled out in 2017. With plans to deploy the initiatives’ next phase at a critical moment, Westphal and Plews-Ogan believe the program will begin to meet some of the needs of an exhausted workforce.
Though terms like “training” and “resilience” trigger many who work in healthcare, nurse manager Austin urges his colleagues not to dismiss the program’s power as “just another class.”
“I don’t want people to roll their eyes and say, ‘Oh, not another training session,’ because it’s not,” he said. “No, it doesn’t appeal to everybody, but it’s a great tool to have in your tool belt to help support you and your team. Give it a chance; it’ll help you. I promise.”
###
Learn about stress injuries, and the Stress First Aid approach; explore UVA Health's Wisdom & Wellbeing web site for team-building resources and an immediate help-line; Watch "Breaking the Silence," a film about mental illness and suicide among healthcare staff; and peruse the Compassionate Care Initiative's regular roster of in-person and virtual activities to build individual coping.
