Tailored Approach Puts Cervical Cancer in the Crosshairs


 If there’s a single truth that associate professor Emma Mitchell knows from 10 years of fighting cervical cancer, it’s this: tailored approaches work.
If there’s a single truth that associate professor Emma Mitchell knows from 10 years of fighting cervical cancer, it’s this: tailored approaches work.
They work in rural areas, like Southwest Virginia, where cervical cancer mortality is two- to three-times higher than elsewhere in the state. They work in global settings where stigma and access inhibit preventative care and curative treatment. And, cemented by long-forged relationships, they work during pandemics.
Over the last decade, Mitchell’s connectedness to Nicaragua—home to the Central American and Caribbean region’s highest cervical cancer mortality rates—has forged alliances with a fantastic array of colleagues. She’s well-known in the region, to Nicaragua’s Ministry of Health authorities, at the two universities on the Caribbean coast, and a familiar face and name to the dozens of clinicians who staff clinics and rural health outposts in communities in and around the city of Bluefields.
VIDEO: No More Lost to Follow-Up
It’s in Bluefields where Mitchell and partner Rebecca Dillingham, an infectious diseases expert, professor of Medicine, and director of UVA’s Center for Global Health Equity, focused cervical cancer in their crosshairs, developing nuanced systems to screen, follow up, and treat patients who’d developed cervical cancer, which is caused by high-risk genotypes of the human papilloma virus (HPV).
“These aren’t processes that occur overnight; they’re not processes that occur when someone from UVA flies to a place and says, ‘This is how you do it.’ You figure out how to do it by taking the time to understand what’s happening, know what partners want to happen next, and how that can be achieved.”
Becca Dillingham, MD, research partner to associate prof. Emma Mitchell, a nurse scientist who studies cervical cancer
It also works.
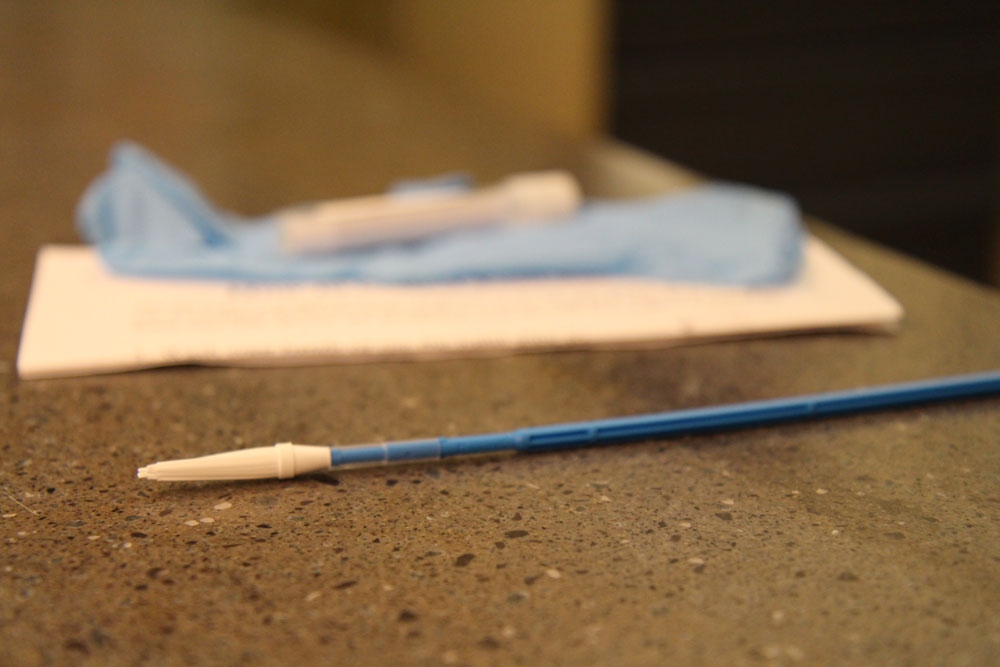
When the pandemic struck, Mitchell’s project infrastructure was largely in place: a local lab to process and diagnose self-collection samples, a method to feed data into Nicaragua’s National Cancer Surveillance System, a protocol for following up with HPV-positive women, and trainings for rural gynecologists to remove cervical cancer lesions using a smartphone based colposcope, a low-cost cervical simulator, and a mobile thermo-ablation machine. So, in spring 2020, when nearly 2,000 HPV self-collection kits were received during the first phase of Mitchell’s pilot study, over 350 HPV-positive women were quickly notified, connected with resources, and urged to take the next steps for treatment. In a moment when the pandemic might have derailed cervical cancer detection and treatment, the vast majority of women with cancerous lesions were treated.




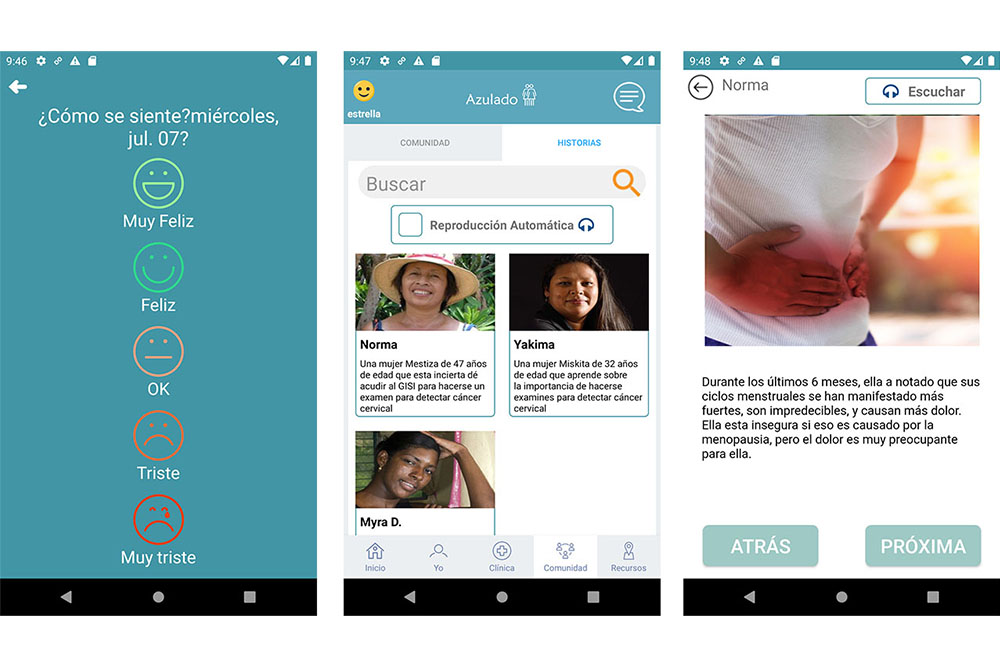

The new smartphone app—which debuted in spring 2021—is the critical final piece of Mitchell’s tailored approach. It provides a roadmap and ethos for other resource-limited countries battling cervical cancer looking for best practices, important as the World Health Organization aims to eradicate cervical cancer in the next century.
But while cool tech often gets props, Dillingham insists the study’s success is built on the partnerships and mutual respect Mitchell has built over time.
“We’re modeling the kind of collaboration that’s essential for true change to occur,” Dillingham said. “These aren’t processes that occur overnight; they’re not processes that occur when someone from UVA flies to a place and says, ‘This is how you do it.’ You figure out how to do it by taking the time to understand what’s happening, know what partners want to happen next, and how that can be achieved.”
Mitchell and her development team continue to refine and tailor the app, and, pending funding, plan to expand screening, treatment, and deployment to communities surrounding Bluefields.
From the Fall 2021 Virginia Nursing Legacy.
